
The eye is principally divided into two separate compartments, the front or ‘anterior chamber’ which is filled with aqueous fluid, and the back or ‘posterior chamber’ which is filled with vitreous gel. When you are born this vitreous gel fills the whole posterior chamber of the eye and is glued to the lining of the eye, including the retina and optic nerve. As we all age this vitreous gel slowly dissolves and shrinks. Eventually the gel completely separates from the back of the eye. This is known as a posterior vitreous detachment (PVD). This is a normal process and occurs in everyone!
In some people the vitreous gel is abnormally sticky, and is very adherent to the central retina, known as the macula. As the gel shrinks, instead of pulling free from the macula (known as a PVD), it stretches the macula. This causes the retina to be swollen or distorted. The corresponding blur and distortion of vision is known as vitreomacular traction (VMT).
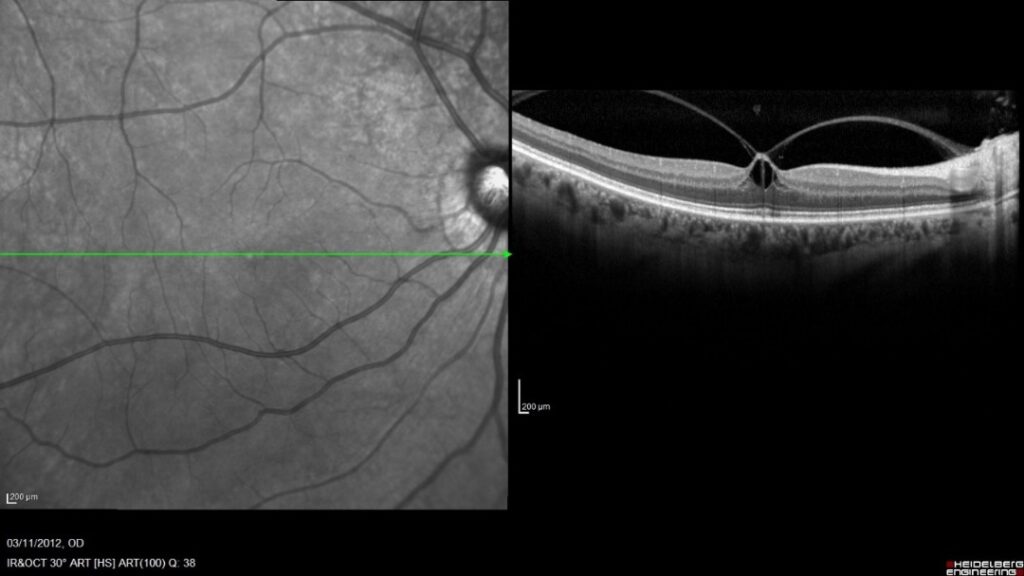
Vitreomacular traction (VMT). This OCT image shows a photograph of the retina on the left, and a cross-section through the retina (at the green line) on the right. This shows how the vitreous gel is pulling away from the retina, but is adherent in the middle, causing stretching or tenting-up of the retina.
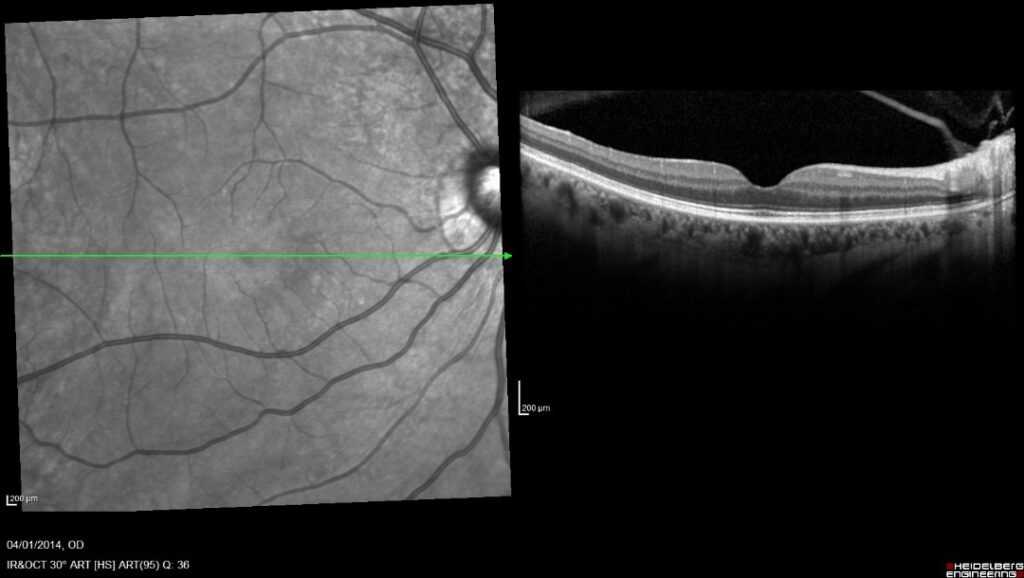
This photograph is from the same patient as above, and shows spontaneous resolution of the VMT, with the vitreous gel separating from the retina, leaving a normal retinal appearance, with a central dip at the fovea (central focal point of the eye).
Vitreomacular traction causes blurred and distorted vision. There are a number of possible outcomes at this stage. Either it will continue to pull on the macular and causing continued or increasing blur and distortion, it may resolve completely on its own, or it may develop into a rip, known as a macular hole (see below).
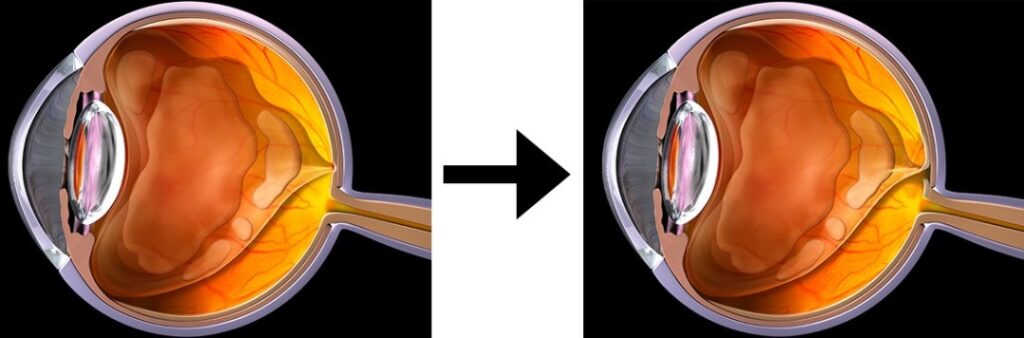
Vitreous separates from the retina and optic nerve but is still attached to the central macular. Over time this may rip the macular, causing a macular hole.

A photograph and corresponding OCT of a macular hole. In the OCT on the right the vitreous has lifted off from the retina, but has torn a small piece of tissue from the retina, creating a full thickness hole in the retina.
How is VMT treated?
During the early stages of VMT there is the potential to for the traction to resolve or be treated and for all vision to return. However, VMT does damage the retina to varying degrees, and sometimes of resolution of the VMT there may be some mild permanent visual impairment.
If a macular hole develops, this will cause immediate profound loss of central vision and not all of this can be restored with surgery.
Usually, if the vision is still good with minimal distortion, VMT could just be observed for signs of deterioration or resolution. If you are very symptomatic, or the symptoms are progressive, there are two principal treatments. One is a straightforward injection into the eye of an enzyme that dissolves the vitreous, thereby releasing the traction. This has an approximate 25-35 % success rate. However, if this treatment fails then the only other option is a vitrectomy.
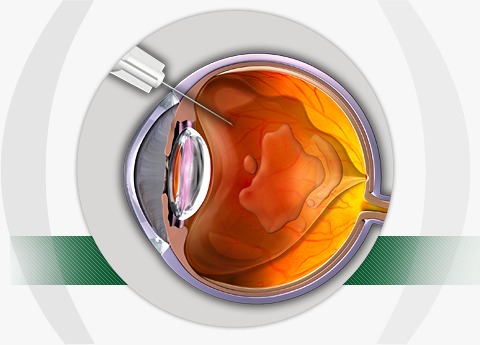
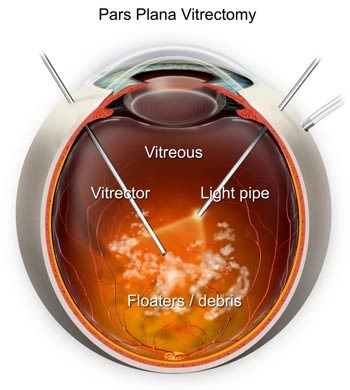
A vitrectomy is an operation to remove the vitreous gel. This is a daycase procedure where you are awake, it takes 20 minutes, and requires no stiches. A vitrectomy has >95% success rate but carries with it a small risk of surgical or post-operative complications that can be associated with any surgery.
Epiretinal membrane
An epiretinal membrane is part of the spectrum of conditions of abnormal macular vitreoretinal adhesion, just as is vitreomacular traction and macular holes are. As with vitreomacular traction and macular holes, the vitreous shrinks with age and tries to separate from the back of the eye, called posterior vitreous detachment (PVD). This is a normal age-related process.
Due to abnormal adhesion between the vitreous and macula, this process creates inflammation of the retina, and causes the deposition of a layer of scar tissue over the surface of the retina. This layer of scarring is known as an epiretinal membrane (ERM).
In its early stages this may be asymptomatic, and can be known as ‘cellophane maculopathy’. However, over time this ERM may progress, even after the PVD has developed. The membrane can become thicker, and begins to shrink. This shrinkage causes the underlying retina to be displaced, start to swell, and become wrinkled. The retina, being the photographic film of the eye will thus start to experience blurring and distortion of images. This wrinkling and distortion sometimes means epiretinal membranes can be referred to as ‘macular pucker’.
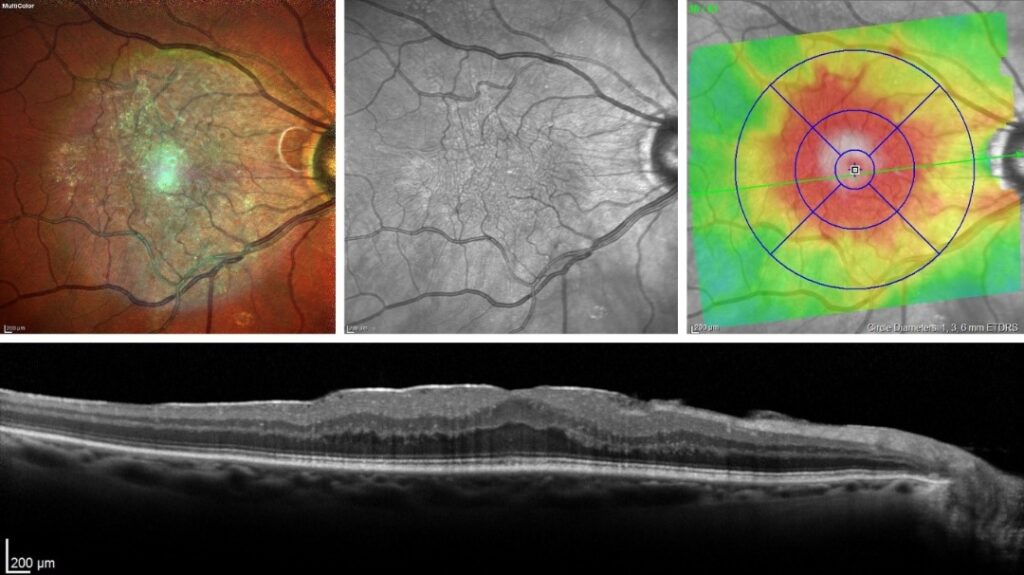
A colour photograph of a retina showing a sheen over the macula. In black and white the wrinkling of the retina is evident. The right hand coloured overlay shows how much swelling there is of the retina. An OCT scan, showing a cross-section of the retina, reveals a thin white line on top of the retina with subtle swelling of the retina.
There are a number of treatment options for epiretinal membranes. If the membrane is mild, meaning the patient does not usually notice blur or distortion, then the membrane can be simply observed. Should the membrane get progressively worse, causing more constant or troublesome symptoms of blur and distortion then the membrane can be peeled away with surgery.
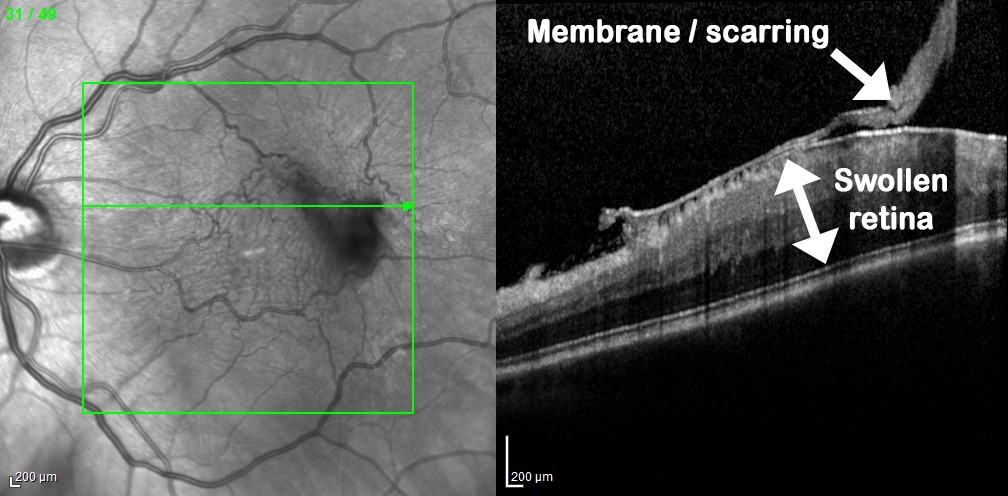
This is a case of more severe swelling and wrinkling caused by an epiretinal membrane, with obvious distortion on the photograph and a thick band of scarring clearly evident on OCT cross-section.
Surgery for epiretinal membranes is a day case procedure known as a vitrectomy. During the operation the ERM is peeled away with a pair of fine micro-forceps. The process of peeling this adherent membrane away is a traumatic one for the retina. Thus, after surgery the vision is often worse for a couple of weeks, and then slowly improves after this. Visual blur and distortion takes months to settle. Most vision comes back over 3 to 4 months, however, vision will continue to improve beyond 1 year. As with all surgery, there are risks to surgery, and 1 in 20 people may have slightly worse blur or distortion after epiretinal membrane surgery.
