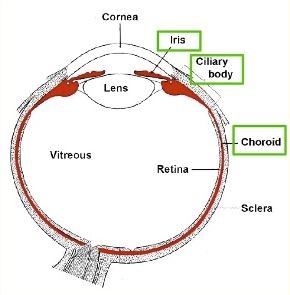
The eye is lined by a thin layer of black pigmentation which absorbs stray light. This layer forms the back of the iris and is a continuous sheet that extends from the back of the iris, covers the ciliary body, and wall of the eye behind the retina (choroid). This layer is called the uvea.
This uvea is composed of closely packed cells with tight junctions between them. The layer effectively acts as a waterproof barrier inside the eye. This forms what is known as a blood-ocular barrier. When this eye barrier is compromised for any reason, inflammatory white blood cells can break through this pigment layer, and cause inflammation inside the eye. When the front section of the eye is inflamed this is known as ‘anterior uveitis’ or ‘iritis’, and white blood cells can be seen in the front section of the eye. When the ciliary body and pars plana are inflamed this is known as intermediate uveitis, and white blood cells can be seen in the anterior vitreous or on the pars plana. When the retinal pigment beneath the retina is inflamed this is known as posterior uveitis, and white blood cells can be seen in the vitreous and retina of the eye. When the whole eye is inflamed this is termed pan-uveitis.

Anterior uveitis. A red eye with a hazy view of iris, an irregular pupil, and white deposits on the inside of the cornea (collections of inflammatory white blood cells).
Inflammation is a process that is often useful for the body to fight infection or repair after injury, however, excessive inflammation can be destructive. For example, rheumatoid arthritis is excessive inflammation of the joints that is destructive to the joints, resulting in limitation of movement and pain. In the same way, excessive inflammation of the eye can cause pain, photophobia, loss of vision, high or low eye pressure, cataracts, and retinal detachments.
There are many causes of uveitis, the most common being unknown (idiopathic). Other causes include genetic causes, such as having the HLAB27 gene, sarcoidosis, rheumatoid arthritis, lupus, Fuchs uveitis, trauma or infection, etc.
The treatment of uveitis is usually to look for an identifiable cause and to treat this. If there is no treatable cause then anti-inflammatory medication can be given, such as steroidal or non-steroidal drops, oral steroids, or oral immunosuppression.
