What are cataracts?
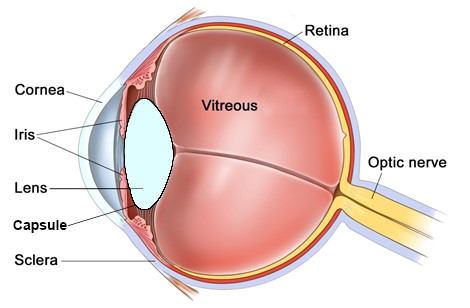
Just as there is a lens in glasses to focus, there is a lens inside the eye to focus. When you are born this lens is clear and elastic, and changes shape to bring images into sharp focus onto the retina (photographic film of the eye). As you age, the natural lens of the eye stiffens, and is less able to focus for near tasks such as reading. This usually occurs in the mid 40’s, and reading glasses are required after this. This stiffening of the lens is known as presbyopia. Eventually, after many years, the lens starts to become cloudy. A cloudy lens is known as a cataract. In the early stages of cataract most people would not even notice a problem with their vision. These early cataracts are often noticed by optometrists or ophthalmologists, but are infrequently discussed. Over time, as the lens becomes cloudier, the vision becomes noticeably blurred. This blur cannot be corrected with glasses. Cataracts also scatter light entering the eye, and commonly give rise to symptoms of glare or photophobia, especially noticeable at night with oncoming car headlights.
Cataracts, just like other aging changes, are a normal and natural part of aging. Everybody will develop a cataract if they live long enough. The age at which cataracts develop is variable. Once a cataract has formed, the only way to improve the vision is with a cataract operation. This is where the old cloudy lens is removed and a new clear acrylic lens is implanted. Without surgery the vision will deteriorate until you cannot perform day to day tasks.
Just as there is a risk of accidental injury with poor sight, there is a risk associated with surgery. For this reason, eye care professionals often talk about cataracts needing to ‘ripen’. This simply means that if the cataract is not causing any visual symptoms then it is not worth any risk to treat them. In contrast, if the cataract is sufficiently noticeable to affect day to day life, then surgery may be worth a small risk to improve the vision.
The risk of cataract surgery is very low. Large national surveys tell us that 95% of patients have improved vision after cataract surgery, 2.5% do not notice an improvement, and 2.5% can be slightly worse. One person in one thousand can be blinded by surgery.
What does cataract surgery involve?
Cataract surgery is a modern day case procedure. Patients usually arrive 1 hour prior to surgery. The nurse checks your details, medical history, and blood pressure and instills dilating eye drops. You will also see the surgeon to answer any final questions and to confirm that you are happy to proceed with surgery by signing the consent form.
With your normal clothes on you are then taken around to theatre where your eye will be anaesthetized using just eye drops. The eye will be cleaned, a drape (sterile sheet) will be stuck to the skin around the eye to keep it clean. This is a large sheet that will cover the face. It will be held off of the nose and mouth by an oxygen bar. The eye will be held open with a clip and the operation started. The operation takes 10-15 minutes. During the operation you will be asked to look directly at a bright light from the operating microscope. This dazzles the vision and so you will only see vague shadows (the other eye is covered up by the drape). After surgery the eye does not need a dressing. You will be given eye drops to instill at home 4 times per day for up to 4 weeks. Your vision will improve the next day, and continue to improve for a few days after this.
If you have cataracts in both eyes, surgery will be carried out sequentially, i.e. 1-2 weeks apart. This gives the first eye time to heal and your vision to return before embarking on a procedure in the other eye.
Will I need glasses afterwards?
The aim of cataract surgery to improve vision and reduce dependence on glasses. When the cloudy cataractous lens is removed it is replaced with a clear plastic lens. This is called an intraocular implant, or intraocular lens (IOL). The IOL required to correct your vision is determined from measurements taken pre-operatively. Thus, most people will not need glasses for distance vision after surgery, but a minor prescription can often eek out extra sharpness from the eye.
The ability to read after cataract surgery is dependent on the type of lens implant (IOL) that is inserted in your eye at the time of surgery. Standard monofocal implants, the only implants available on the NHS, provide quality distance vision only. Reading or intermediate glasses will always be required for near tasks.
Premium implants, such as presbyopic or toric implants are only available to private patients. Presbyopic implants, also known as multifocal implants, can give you clear vision for distance and reading. Presbyopic implants are not necessarily better than the standard monofocal lenses, but offer less dependence on glasses for close work. Both types of lenses have pros and cons. The monofocal implants gives the sharpest vision with the least side-effects. Presbyopic implants give a good range to the focus but sacrifice very slightly some sharpness and contrast, and can sometimes cause some ghosting or glare under certain lighting conditions. For this reason people talk of multifocal lenses requiring a period of neural adaptation, whereby your brain gets used to these nuances, until your vision is accepted as “normal” for you. This may take some months. 1 in 100 people never adapt to these lenses and the lenses have to be removed and replaced with monofocal lenses. Additionally, whilst 70% of the time you will not require reading glasses, 30% of the time reading glasses may still be helpful or required, especially for small print or reading with poor lighting.
Toric IOLs correct astigmatism. Astigmatism is the irregular curvature of the eye, where the eye is rugby ball shaped rather than football shaped. Astigmatism therefore causes blurred and distorted vision. Astigmatism is usually corrected with glasses or contact lenses. When you have cataract surgery you have a golden opportunity to correct this astigmatism with a toric IOL, thereby reducing your dependence on glasses after surgery. Toric IOLs can be monofocal or multifocal in design.
The type of lens implant that you should have depends on your visual requirements, eye measurements, and your expectations from surgery. You should discuss this with your ophthalmologist.
How long will the implant last?
The intraocular lens (IOL) is made of acrylic and will never become cloudy or degrade. However, with time, a film can form on the back surface of the lens that may start to blur the vision. This condition is called posterior capsule opacification (PCO). PCO is not clouding of the lens, but a cloudy membrane behind the lens. It can be easily treated in clinic if it occurs. A painless 5 minute laser procedure in clinic will eliminate it permanently.
Complicated Cataract (weak zonules, dislocated lens)
The natural lens of the eye is contained within an elastic ‘capsular bag’. This bag is suspended within the eye by a series of ‘guy ropes’ around the outside of the lens called zonules. This is rather like a trampoline being suspended by springs all around its edge, holding the trampoline taut and central.
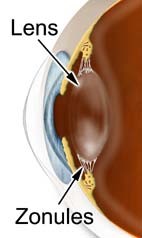
In some individuals these zonules can be naturally weak, especially if the cataract is very dense. In others these zonules may have been damaged by trauma, previous surgery, or a condition known as pseudoexfoliation. In these circumstances the lens or cataract of the eye may dislocate spontaneously, without any injury, or even dislocate unexpectedly during cataract surgery. If this occurs then the lens of the eye, instead of being suspended near the front of the eye, may fall into the vitreous gel at the back of the eye, or alternatively, let the vitreous gel at the back of the eye come forwards into the front of the eye. This type of dislocated lens or vitreous migration can not be repaired with conventional cataract surgery. This requires a retinal surgeon to remove the vitreous gel and the lens / cataract using completely different equipment to that used during cataract surgery. This procedure is known as a ‘vitrectomy’.

High magnification view through an iris showing the curcular pupil, with a decentered / dislocated cataractous lens. This is due to weak zonules.
Similarly, 2% of all cataract operations have a complication known as ‘posterior capsule rupture’. This is where the capsular bag that holds the lens in position splits during surgery, allowing the cataract or lens to potentially fall into the vitreous gel of the eye, or allowing the gel to come forward. Again, this can only be repaired by a retinal surgeon with a vitrectomy procedure.
