The Eye
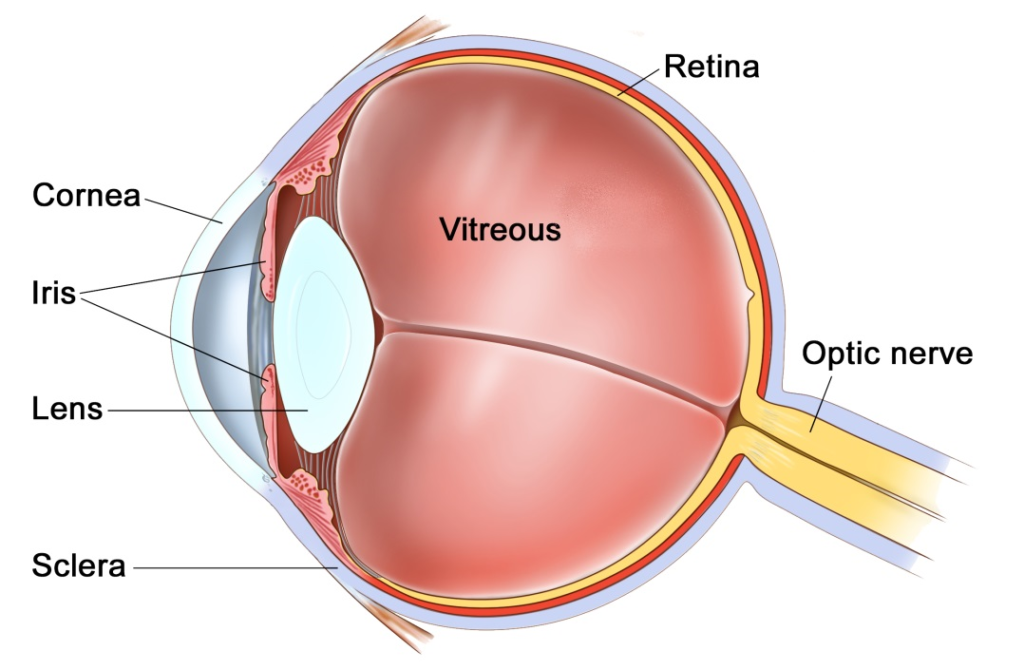
The eye is like a camera, with a lens at the front to focus light, and a film at the back to capture an image. The photographic film of the eye is known as the retina. In between the lens and the retina, the eye is filled with a gel, known as vitreous.
The vitreous gel was important during development of the eye where it acted as a scaffold for blood vessels. After birth the gel is no longer required and gradually liquefies and shrinks in size. Inevitably, usually after 40 years or more, the gel has shrunk so much that it can no longer completely fill the cavity of the eye. At this point the vitreous gel separates from the retina in a process known as a ‘posterior vitreous detachment’ or ‘PVD’. This is a natural process and occurs in everybody with time.
As with many conditions, this natural process can occasionally go wrong resulting in a range of medical conditions, such as floaters, vitreous haemorrhage, detached retina, epiretinal membrane, or macular hole. These conditions alter the focus of light entering the eye and cause blurred vision.
What is a retinal detachment?
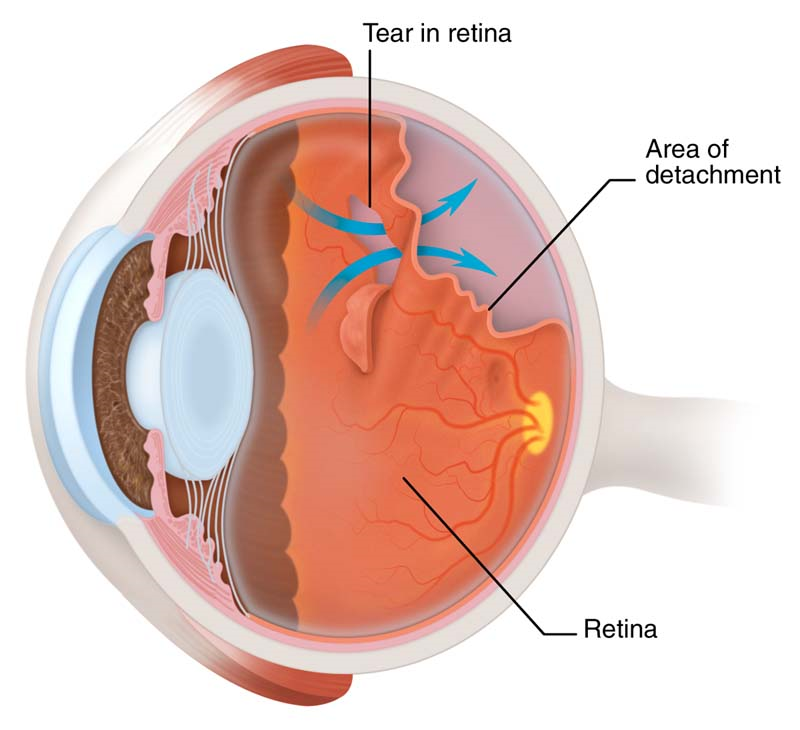
A retinal detachment is when the photographic lining of the eye begins to peel away from the wall of the eye. An analogy often used is wall-paper peeling away from a wall. In most cases the retina detaches because a hole or a tear has formed in the retina allowing fluid to pass underneath the retina. The tear in the retina is usually the result of the age-related posterior vitreous detachment mentioned above. Certain people are at higher risk of detachments than others. These include people who are short sighted, those who have had cataract surgery, particularly complicated cataract surgery, and those who have suffered a direct blow to the eye. Some types of retinal detachments can run in families but these are rare.
What are the symptoms of a retinal detachment?
Retinal detachments are initiated by tears in the retina. The retina is very vascular and bleeds when it tears. Thus, the symptoms of a torn retina are a sudden increase in floaters described as a “shower of floaters”. Days to weeks later a curtain-like blurred patch or shadow appears in the peripheral vision. This slowly enlarges. If the detachment is allowed to reach the central retina, known as the macula, then the vision will become significantly blurred and distorted. If this occurs, some of the visual loss will be permanent. It is important to try and repair the detachment early to prevent this loss of vision.
Do I need to have the detachment repaired?
Without repair the entire retina will detach and the eye will become blind. The sooner the retina is repaired the better the visual outcome is likely to be. If the detachment is small, and the vision still good, this is termed a macular-on detachment. We like to repair macular-on detachments within 24 hours. If the vision is reduced due to a large detachment, some vision will already have been lost, this is termed a macular-off detachment. Macular-off detachments have already lost some vision permanently and a delay of a few days does not affect the final outcome. We like to repair macular-off detachments within 5 days for the best visual outcomes.
How is the retinal detachment repaired?
To repair the retina we first need to remove the cause of the detachment, the vitreous gel, in an operation called a vitrectomy. The retina is then flattened by removing the fluid from under the retina, the tear in the retina is sealed with either laser or cryotherapy, and the eye is filled with an internal bandage known as a tamponade. The tamponade is usually a bubble of gas, but in advanced cases it may be a bubble of silicone oil. This bubble holds the retina flat against the wall of the eye whilst it heals. Any gas in the eye will slowly dissolve after the operation. Depending on the gas used, the gas may last as little as 1 week for air, 3 weeks for sulphur hexafluoride (SF6), or up to 8 weeks for perfluoropropane (C3F8). Oil does not dissolve and needs to be removed with a second procedure.
The operation is usually performed as a day case procedure, whilst you are awake, but can also be done at request with you asleep, under sedation or general anaesthetic. The whole procedure takes approximately 30 minutes. After the procedure you have a patch on the eye for 1 night, and drops for 1 month.
What is the success rate?
Retinal detachments are fixed in 85% of cases with a single procedure. 15% of cases redetach and need further repair. Some people may require several operations. In 5% of cases the retina can not be saved and the eye will be blind.
Are there any risks?
All operations carry some risk, however, without surgery the eye will be permanently and totally blind. Compared to blindness the risks are relatively insignificant. One in 1000 can be blinded by infection or haemorrhage within the wall of the eye, 15% will redetach and need further surgery. Some people can have raised pressure or glaucoma which may be permanent.
If you have not had cataract surgery, then all patients within 1-2 years of surgery will develop a cataract. Cataracts are a cloudy lens in the eye that blurs the vision and cannot be corrected with glasses. Cataracts are a normal natural part of aging, and most people will require cataract surgery in their lifetime anyway. The cataract can be removed if and when it becomes visually significant.
The recovery
Immediately after your procedure we may ask you to posture on one side or another, or face down to the floor for a couple of hours. Subsequently, you may have some instructions on which side to sleep on at night for 1-2 weeks.
When you go home after your procedure you will be given a bottle to drops to apply 4 times per day for 4 weeks. This drops contains both antibiotic and anti-inflammatory medications. Typically patients are seen at 1 day, 2 weeks and 2 months post-operatively.
You will not be able to fly if you have a gas tamponade in the eye until the tamponade has dissolved. If you have a general anaesthetic with a gas tamponade you must tell your anaesthetist that you have gas in the eye. Flying and anaesthetics are not a problem if you have a silicone oil tamponade.
We generally advise you to have 1-2 weeks off of work and not to swim for 2 weeks.
Where can I find more information?
https://www.nei.nih.gov/health/retinaldetach/retinaldetach
http://www.moorfields.nhs.uk/condition/retinal-detachment
http://en.wikipedia.org/wiki/Retinal_detachment
http://www.nhs.uk/conditions/Retinal-detachment/Pages/Introduction.aspx
Important information
After your operation your sight should gradually improve and the eye feel more comfortable. If at any stage during your recovery you feel that the eye is becoming more painful, or the sight worse, then you must call for advice. Do not wait for your appointment.
Useful Telephone Numbers
Mr Steven Harsum’s Private Secretary 0207 112 8246
Ashtead Hospital 01372 221 400
Optegra (Surrey) Eye Hospital 01483 903 004
St Anthony’s Hospital 0208 337 6691
Emergencies:
Monday to Friday – St Helier Eye Casualty: 0208 296 3817
Evening/Weekend – Moorfields at St Georges: 020 8725 2064
