- Corneal Degeneration (Dystrophy)
The front surface of the eye is a clear window known as the cornea. It is 0.5mm thick in the centre and 1mm thick at the periphery. It is a 3 layer structure. On the front surface it has a thin epithelium, in the middle it has a thick stroma, and on the back / inside surface it has a thin endothelium. Behind the cornea sits the aqueous, iris and pupil.
Any of the 3 layers of the cornea can become weakened or degenerative. The commonest abnormalities are Keratoconus and Fuchs endothelial dystrophy.
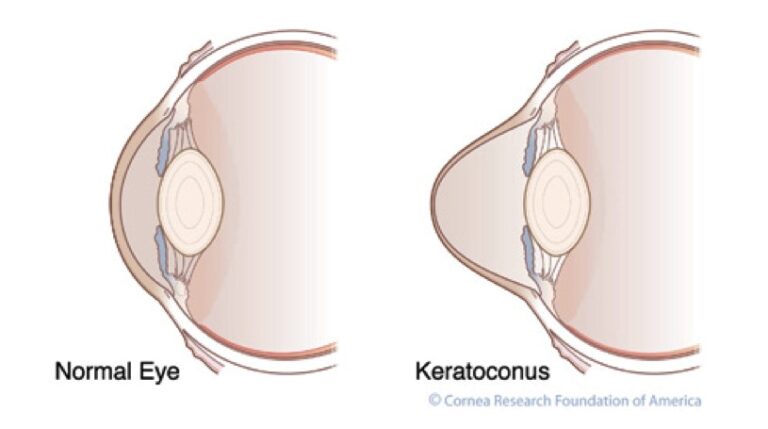
Keratoconus is a gradual thinning of the stroma of the cornea of both eyes. This reduces it structural integrity and results in a gradual change of shape over months to years. This results in a rapidly changing prescription with increasing astigmatism. Initially this can be managed with glasses, but as the thinning progresses, rigid contact lenses may be required to keep the focus. Further progression requires surgical intervention in the form of collagen crosslinking, INTACs, partial or full thickness corneal grafting.
Note how in Keratoconus the normal cornea looses its shape and becomes distorted.
Fuchs dystrophy is a degeneration of the endothelium (lining) of the cornea of both eyes. The endothelial cells are responsible for keeping the corneal healthy and transparent. In the early stages of Fuchs the patient usually has no symptoms. As the condition progresses, the cornea can loose its transparency, resulting in gradual loss of vision. This may be manageable with hypertonic saline drops initially, but as the condition progresses, an endothelial partial thickness graft from cadaveric eyes may be required.
These corneal dystrophies can be detected by an ophthalmologist. If they are discovered then this will affect any planned eye surgery, such as refractive laser surgery or cataract surgery.
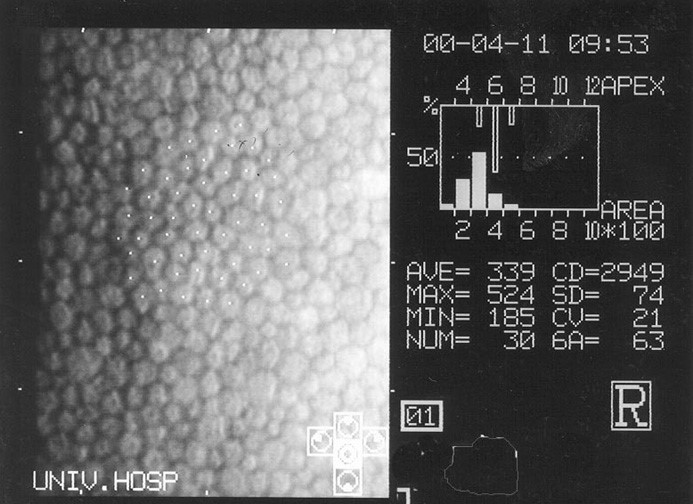
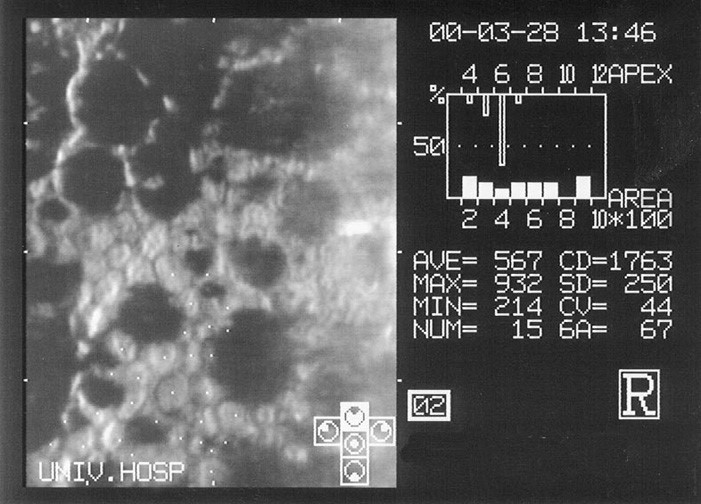
Endothelial cells in Fuchs dystrophy showing reduced number of cells, larger irregular cells, and gaps where no cells are visible, known as guttate.
