- Diabetic Retinopathy & Maculopathy
Diabetic retinopathy.
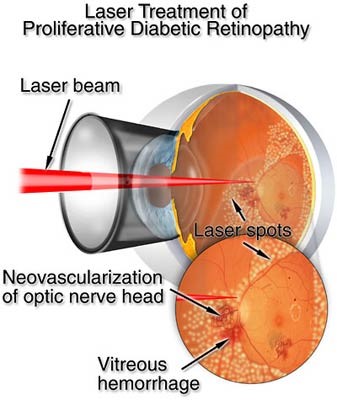
The retina is the photographic film of the eye. It is very vascular and filled with fine capillaries supplying it with oxygen. In diabetic retinopathy, these capillaries become damaged by fluctuations in blood sugar, such that they begin to disappear. Once the capillaries have gone they never grow back, i.e the retina is permanently damaged. Without capillaries the retina does not get any oxygen, and so the retina swells and degenerates. The retina is effectively ischaemic. In response to ischaemia the retina releases growth factors known as vascular endothelial derived growth factors (VEGF). If enough of the retina is devoid of oxygen, as the VEGF levels rise, the whole eye can start to develop random new blood vessels. These abnormal ‘new vessels’ are destructive, rather like the roots of some plants are to walls. They grow into the iris and drainage system of the eye and cause glaucoma, they grow into the vitreous and cause a vitreous haemorrhage, they grow between the retina, optic nerve and vitreous and cause tractional retinal detachments. This is known as proliferative retinopathy. If these ‘new vessels’ are untreated the bleeding, scarring and glaucoma blind the eye permanently.
Diabetic retinopathy.
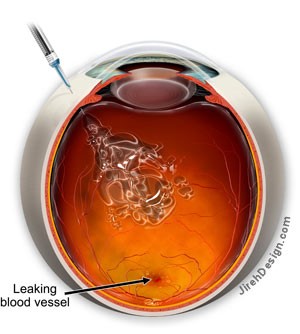
In diabetic maculopathy, fluctuations in blood sugar cause damage to the fine capillaries that supply oxygen to the macula. The macula is the area of retina that supplies the finest vision, required to see detail and to read. Damage to these capillaries makes them become leaky. Fluid normally held within blood vessels, leaks out into the macula, causing it to swell. As the retina swells the vision becomes increasingly impaired. As with retinopathy, some capillaries disappear permanently, and the macula can become ischaemic. Increasing swelling and ischaemia of the macula slowly cause permanent damage to the vision.
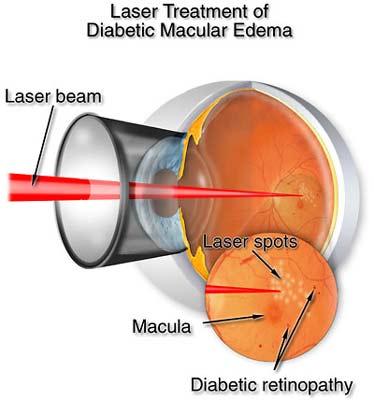
Macular laser is much more subtle that PRP laser (for proliferative retinopathy). Macular laser is designed to stimulate the retina and encourage it to dry out. The laser can take 6 months to show any benefit, and is therefore often reserved for patients with maculopathy that have normal sight. Macular laser is designed to prevent loss of vision, not to improve vision.
Intravitreal anti-VEGF injections, known as either Avastin (Bevacizimab), Lucentis (Ranibizumab) or Eylea (aflibercept), are for when the vision has already deteriorated, and the central macular is involved. They work more quickly than laser and reduce the leakage of blood vessels, drying the macula. Anti-VEGF drugs can improve vision in 40% and reduce the risk of visual loss in the rest. 4% continue to lose vision regardless of treatment.